The Wnt signaling pathway has emerged as a cornerstone in the field of organ regeneration, offering tantalizing clues into how tissues repair and renew themselves. This ancient and evolutionarily conserved pathway plays a pivotal role in embryonic development, but its reactivation in adult tissues holds the key to unlocking regenerative potential. Researchers are now delving deep into the molecular intricacies of Wnt signaling, hoping to harness its power for therapeutic applications. From the regrowth of liver tissue to the repair of heart muscle, the implications are profound and far-reaching.
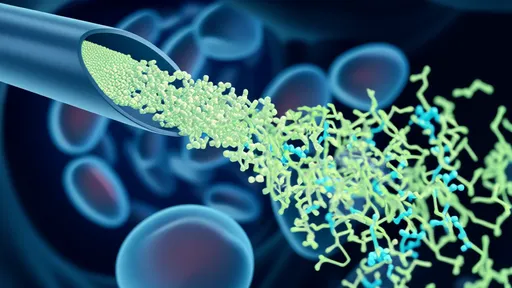
At the heart of Wnt signaling lies a complex interplay of proteins that dictate cellular behavior. When a Wnt ligand binds to its receptor, it sets off a cascade of events that can lead to cell proliferation, differentiation, or even self-renewal. The pathway is typically divided into two branches: the canonical (β-catenin-dependent) and non-canonical (β-catenin-independent) routes. Each branch exerts distinct yet sometimes overlapping effects on tissue regeneration. For instance, the canonical pathway is often associated with driving progenitor cells to multiply, while the non-canonical arm influences cell migration and polarity—both critical for rebuilding damaged structures.
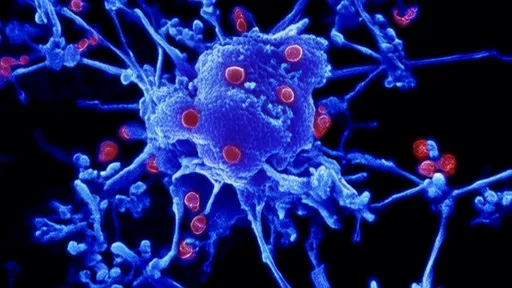
One of the most striking examples of Wnt-driven regeneration comes from the animal kingdom. Certain species, like zebrafish and salamanders, exhibit remarkable regenerative abilities, capable of regrowing entire limbs or organs with near-perfect fidelity. Studies have shown that Wnt signaling is reactivated during these processes, acting as a molecular switch that turns on regenerative programs. In zebrafish, for example, inhibition of Wnt signaling disrupts fin regeneration, while its activation accelerates the process. These findings suggest that the pathway is not just a passive player but an active orchestrator of regeneration.
In mammals, the story is more nuanced but no less compelling. While humans and other mammals have limited regenerative capacities compared to zebrafish, certain tissues—such as the liver and skin—retain a degree of regenerative prowess. The liver, in particular, can regenerate up to 70% of its mass within weeks, a feat largely attributed to the reactivation of developmental pathways, including Wnt. Hepatocytes, the liver's primary functional cells, re-enter the cell cycle and proliferate under the guidance of Wnt signals. However, chronic activation of Wnt can lead to fibrosis or cancer, highlighting the delicate balance required for therapeutic intervention.
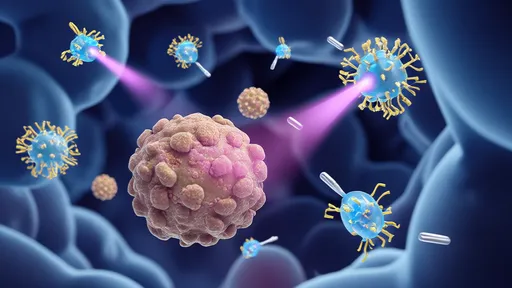
The potential for targeting Wnt signaling in regenerative medicine is immense but fraught with challenges. On one hand, activating the pathway could stimulate tissue repair in conditions like myocardial infarction or chronic wounds. On the other, unchecked Wnt activity is a hallmark of many cancers, necessitating precise control over its modulation. Researchers are exploring various strategies, from small-molecule inhibitors to gene therapies, to fine-tune Wnt signaling in a context-dependent manner. For instance, timed delivery of Wnt agonists following injury might jumpstart regeneration without tipping the scales toward malignancy.
Recent advances in single-cell sequencing and CRISPR-based technologies have opened new avenues for dissecting Wnt's role in regeneration. Scientists can now track how individual cells respond to Wnt signals during repair, revealing heterogeneity in regenerative potential. Some cells may be primed to proliferate, while others contribute to structural support or immune modulation. This granular understanding could pave the way for personalized regenerative therapies, where Wnt modulation is tailored to specific cell populations or injury types.
Beyond its direct effects on cell behavior, Wnt signaling intersects with other critical pathways involved in regeneration, such as Notch, Hedgehog, and TGF-β. These cross-talk mechanisms create a robust yet flexible network that adapts to different regenerative contexts. For example, in bone repair, Wnt and BMP (a subset of TGF-β) signaling collaborate to promote osteoblast differentiation. Disrupting this interplay can lead to poor healing or ectopic bone formation. Thus, a holistic approach that considers these interactions will be essential for developing effective regenerative therapies.
Ethical and practical considerations also loom large in the pursuit of Wnt-based regeneration. While animal models provide invaluable insights, translating these findings to humans requires rigorous testing for safety and efficacy. Moreover, the long-term consequences of manipulating such a fundamental pathway remain uncertain. Could transient Wnt activation trigger unintended consequences years later? These questions underscore the need for cautious optimism as the field progresses.
Looking ahead, the study of Wnt signaling in organ regeneration stands at a thrilling crossroads. With each discovery, we inch closer to unlocking the body's latent regenerative abilities, potentially revolutionizing how we treat injury and disease. Whether it's repairing a damaged heart or restoring function to a failing liver, the Wnt pathway offers a beacon of hope—one that shines ever brighter as science unravels its secrets.
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025