The concept of a "window of opportunity" in early childhood has gained significant traction in pediatric research, particularly concerning allergy prevention. Emerging evidence suggests that the first few months and years of life represent a critical period during which immune system development can be profoundly influenced. This delicate phase, often referred to as the allergy prevention window, presents healthcare providers and parents with a unique chance to implement strategies that may reduce the likelihood of allergic conditions later in life.
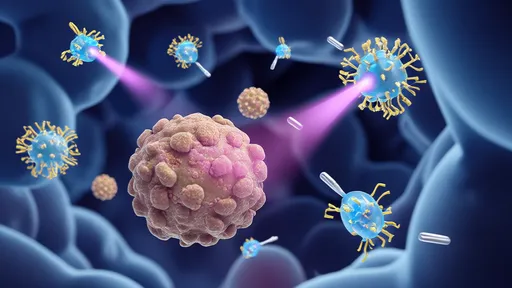
Recent studies have shifted the paradigm around infant feeding practices and environmental exposures. Where previous generations often delayed the introduction of potential allergens, current understanding emphasizes the importance of timely exposure. The developing immune system appears most receptive to establishing tolerance when certain foods are introduced during this specific developmental window, typically between 4-6 months of age for most infants. This approach represents a significant departure from earlier recommendations and continues to evolve as research provides deeper insights into immune maturation processes.
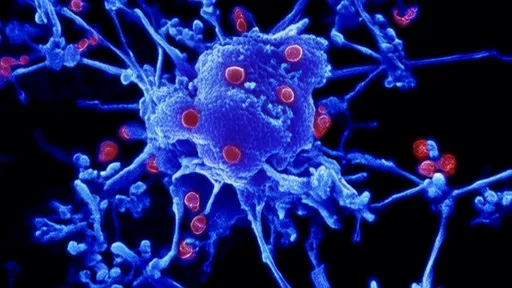
The gut microbiome plays a starring role in this immunological drama. During the first 1000 days of life - from conception through approximately two years of age - the microbial communities establishing themselves in an infant's digestive tract appear to shape immune responses in ways that can either promote or prevent allergic sensitization. Factors influencing this microbial colonization include delivery method, breastfeeding practices, antibiotic exposure, and early dietary patterns. Researchers now believe that optimizing these factors during the critical window may help "program" the immune system toward tolerance rather than hypersensitivity.
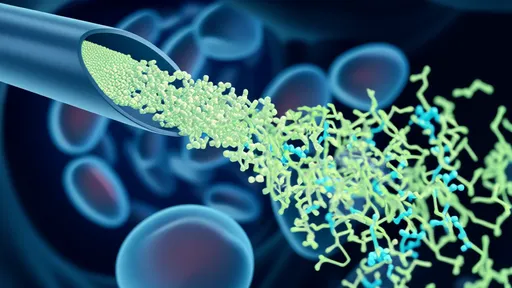
Maternal nutrition during pregnancy and lactation forms the foundation of allergy prevention strategies. Nutrients like omega-3 fatty acids, vitamin D, and various polyphenols appear to cross the placental barrier and later appear in breast milk, potentially influencing fetal and neonatal immune development. While the exact mechanisms remain under investigation, observational studies consistently show associations between maternal dietary patterns during these periods and childhood allergy outcomes. This has led to renewed focus on supporting maternal nutrition as a primary prevention strategy.
Environmental exposures during infancy similarly contribute to immune programming. The so-called "hygiene hypothesis" has evolved into the more nuanced "microbial hypothesis," recognizing that exposure to diverse microorganisms - rather than simply avoiding cleanliness - helps train developing immune systems. Practical applications include encouraging outdoor play, pet ownership, and avoiding excessive sterilization of home environments. These exposures appear most impactful when they occur during the critical prevention window, suggesting timing matters as much as the exposures themselves.
Urbanization and modern lifestyles have inadvertently altered many of the natural exposure patterns that previously shaped immune development. The increasing prevalence of allergic conditions worldwide has paralleled these societal changes, prompting researchers to investigate which modifications might be most protective. Some studies suggest that farm environments, with their rich microbial diversity, may offer particular benefits when experienced during the allergy prevention window. While not practical for all families, understanding these protective mechanisms may lead to more accessible interventions.
Healthcare providers now face the challenge of translating this complex science into practical guidance for families. Personalized approaches that consider family history, environmental factors, and individual risk profiles are replacing one-size-fits-all recommendations. The dynamic nature of research in this field requires clinicians to stay abreast of evolving evidence while helping parents navigate sometimes conflicting information. Shared decision-making models have proven particularly effective in implementing allergy prevention strategies during the critical window.
Monitoring infant responses during the prevention window requires both clinical expertise and parental observation. Early signs of potential allergic tendencies - such as persistent eczema, digestive discomfort, or respiratory symptoms - may indicate the need for adjusted approaches. Emerging technologies, including microbiome analysis and epigenetic testing, may eventually provide more precise tools for assessing individual risk and tailoring interventions. Currently, careful clinical assessment remains the cornerstone of identifying infants who might benefit from specialized prevention strategies.
The long-term implications of interventions during the allergy prevention window continue to unfold through longitudinal studies. Early results suggest that appropriate timing of allergenic food introduction, for instance, may reduce the incidence of peanut and egg allergies by up to 80% in high-risk populations. Similar promising data exists for other allergic conditions, though researchers caution that effects may vary based on genetic predisposition and environmental co-factors. This growing evidence base is reshaping both clinical practice and public health recommendations worldwide.
Disparities in allergy prevalence across populations highlight the complex interplay between genetics, environment, and timing. Children in developed nations experience significantly higher rates of allergic conditions than those in developing countries, even after accounting for diagnostic differences. Research into these variations provides important clues about which aspects of modern life might be modified during the critical prevention window to achieve better outcomes. International collaborative studies are particularly valuable in untangling these complex relationships.
Future directions in allergy prevention research include investigating the potential of targeted probiotics, refined dietary approaches, and precision medicine applications. The recognition of multiple prevention windows - potentially including prenatal, early postnatal, and even preconception periods - adds layers of complexity to this evolving field. As scientific understanding deepens, the challenge lies in translating these insights into practical, equitable strategies that can benefit diverse populations during this critical developmental phase.
Parents navigating the allergy prevention window often face information overload and conflicting advice. Clear communication from healthcare providers about evidence-based strategies becomes essential in this context. Emphasizing the importance of this developmental period while acknowledging individual variations helps families make informed decisions without undue anxiety. Support networks and reliable educational resources play crucial roles in successful implementation of prevention approaches during this formative time.
The economic implications of effective allergy prevention are substantial, considering the lifelong burden of allergic conditions on healthcare systems and quality of life. Investment in research and education surrounding the prevention window may yield significant returns through reduced disease prevalence and severity. Policy makers increasingly recognize the value of early prevention strategies, though translating this recognition into widespread practice remains an ongoing challenge requiring multidisciplinary collaboration.
As the science of allergy prevention continues to advance, the focus on early developmental windows offers hope for reversing the rising tide of allergic conditions. The intricate dance between genes, environment, and timing during this critical period holds keys to understanding immune dysregulation and developing more effective interventions. While many questions remain unanswered, current evidence provides actionable insights that are already changing clinical practice and improving outcomes for countless children worldwide.
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025