For individuals managing hypertension, the way they start their day can significantly impact their blood pressure levels and overall cardiovascular health. Morning routines, particularly the transition from sleep to activity, require careful consideration to avoid sudden spikes in blood pressure. The body undergoes natural changes during the early hours, and understanding how to move safely can make a profound difference.
Waking up gradually is essential for hypertensive patients. Abruptly jumping out of bed can cause a sudden surge in blood pressure, as the body shifts from a state of rest to activity. Instead, taking a few moments to breathe deeply and stretch lightly while still lying down can help the circulatory system adjust. This gentle awakening allows the heart rate and blood pressure to stabilize before standing.
The importance of hydration cannot be overstated when it comes to morning routines for hypertension. Overnight, the body loses fluids through respiration and perspiration, leading to mild dehydration. Drinking a glass of water upon waking helps replenish lost fluids and supports healthy blood viscosity. Lukewarm water is often recommended over cold water, as extreme temperatures can sometimes trigger unnecessary stress responses.
Movement should be introduced slowly and mindfully. Simple seated stretches or ankle rotations can prepare the body for more active movements. Rising from bed should be done with care—first sitting at the edge of the bed for a minute or two, allowing the body to acclimate to an upright position before standing. This is particularly crucial for those who experience orthostatic hypotension, where blood pressure drops suddenly upon standing.
Morning exercise, while beneficial for long-term blood pressure management, should be approached with caution in the early hours. High-intensity workouts immediately after waking may place undue stress on the cardiovascular system. Gentle activities like walking or tai chi are preferable choices for hypertensive individuals in the morning. These low-impact exercises promote circulation without causing dangerous blood pressure fluctuations.
Breathwork plays a pivotal role in regulating morning blood pressure. Practicing slow, diaphragmatic breathing for five to ten minutes upon waking can activate the parasympathetic nervous system, which helps lower blood pressure. This technique counters the natural morning surge in cortisol and adrenaline that contributes to higher blood pressure readings upon awakening.
The timing of medication is another critical factor that intersects with morning movements. Many antihypertensive medications are designed to be taken in the morning to align with the body's natural circadian rhythms. Patients should consult their physicians about the optimal time to take their medication relative to their waking routine and breakfast schedule.
Environmental factors in the bedroom can influence these morning transitions. Maintaining a comfortable room temperature helps prevent blood vessel constriction due to cold. Similarly, ensuring adequate lighting can help the body's natural wake-up process, reducing the shock to the system that sometimes comes with sudden alarms in dark rooms.
Breakfast choices complement these movement strategies for comprehensive blood pressure management. Foods rich in potassium, magnesium, and fiber support healthy blood pressure levels. Avoiding excessive caffeine first thing in the morning may be advisable for some individuals, as it can contribute to temporary blood pressure elevations during the vulnerable morning period.
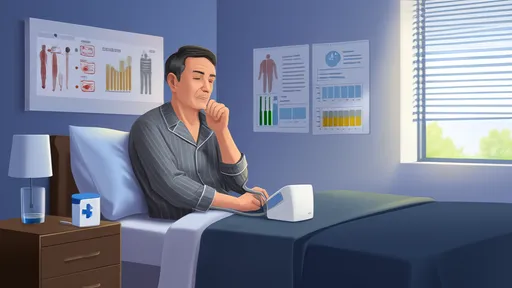
Monitoring blood pressure at consistent times each morning provides valuable feedback about how these routines affect individual physiology. Taking readings after using the bathroom but before breakfast and medication offers the most standardized measurement. This data helps patients and healthcare providers assess the effectiveness of both pharmacological and lifestyle interventions.
Psychological approaches to morning routines matter just as much as physical ones. Starting the day with positive affirmations or brief meditation can set a calm tone that benefits blood pressure regulation. Stress management in these first waking moments creates a foundation for better cardiovascular health throughout the day.
The transition from lying down to standing warrants particular attention. Many hypertensive patients experience their highest blood pressure readings in the first few hours after waking. Using support like bed rails or nearby furniture when first standing can prevent falls that might occur if dizziness or lightheadedness develops during this transition period.
Footwear choices surprisingly factor into morning safety for hypertension patients. Slippers with good support and traction prevent slips while also promoting better circulation than going barefoot. Compression socks may be recommended for some individuals to aid venous return during those initial upright hours.
Temperature regulation extends beyond the bedroom environment. Avoiding extremely hot showers in the morning is advisable, as the heat can cause blood vessels to dilate rapidly, followed by compensatory mechanisms that may stress the cardiovascular system. Warm rather than hot water, with gradual temperature changes, proves safer for hypertensive individuals.
These morning practices don't exist in isolation but rather form part of a holistic approach to blood pressure management. When combined with consistent sleep schedules, stress reduction techniques, and proper medical care, these thoughtful morning movements create a foundation for better cardiovascular health throughout the day.
Individual variation means that not all recommendations will suit every hypertension patient equally. Working with healthcare providers to tailor these morning practices to personal health status, medication regimens, and specific risk factors ensures the safest and most effective approach to managing blood pressure from the moment of waking.
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025
By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025

By /Jul 21, 2025